As appeared in Hartford Business Journal on October 18, 2021.
Author: Lisa Trumble, President and CEO
These days it seems that everyone and every business is talking about healthcare value or value-based care: What is value-based care? Why is it needed? What does it mean to provide value-based care? This discussion wouldn’t be required if our community, employers, and patients were satisfied with the value they are receiving from the healthcare community. But unfortunately, this is not the case.
So how do we define value in healthcare? Value in healthcare represents an improvement in health outcomes (quality and patient experience) relative to the costs for healthcare services. In the US, we pay more for healthcare services than any other high-income earning nations, and we have worse outcomes in terms of mortality, morbidity, and disease burden. So we have to ask ourselves if we are paying more and receiving worse quality, why would we be put up with this? The value-based movement is an intentional approach to improve quality and experience, while reducing the cost of care.
Before COVID, there was significant frustration with the continued escalation of healthcare costs to the point of reaching 18% of GDP, resulting in increased employee contributions, under coverage – or no coverage – and limited access (availability of services or the ability to use services at the appropriate time). Blame was pointed at the provider community for the lack of price and quality transparency and the evil fee-for-service (a payment for each unit of service provided) structure they operate within.
However, much of this criticism failed to acknowledge the many other contributors to this dilemma. Regardless, we can all admit that there is plenty of blame to go around and plenty of change needed. Some of the required changes are clear, e.g., our insurance structure and pharmaceutical costs. However, others are not appreciated or are less visible but contribute in a meaningful way to our problem: lack of accountability and predictability in outcomes and clinical integration (establishing a connection with a complete understanding of the healthcare services provided).






COVID helped us all see the fragility and fragmentation of our healthcare structure. The fee-for-service chassis that so many are dependent upon was unable to sustain the basic foundations of our provider practices and hospital structures. The fragmentation demonstrated no clear accountability for patients within our systems and gaps with the most vulnerable within our communities. With all the challenges, many within our community rose to the occasion to develop the framework for a response and action that was exceptional. We may not face these same challenges during normal times, but it may seem just as critical for many patients whose lives depend on our ability to execute.
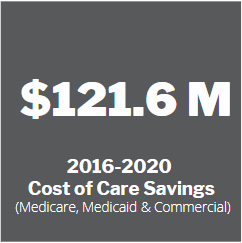
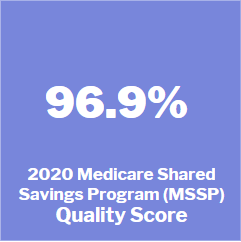
Value-based care is all about seamless execution, efficiency, and effectiveness in the delivery of healthcare. Value-based care is the treatment of the ‘whole person’, including clinical, behavioral, and socio-economic care. It includes targeting the health disparities in the community and population. The results are improved quality, lower costs, and improved health outcomes for individuals and our community. Generating consistent improvements in cost and quality outcomes requires accountability at the provider level, generally with a primary care provider, and a significant degree of clinical integration that eliminates overuse, misuse, or underuse of healthcare resources and mitigates the potential for adverse outcomes.
The reality is without these two critical factors (accountability and integration), all other efforts will fail at addressing the cost and quality problem because utilization (the frequency of services provided) and outcomes will continue in an unmanaged fashion. Value-based care focuses on patient actions and interactions with the expressed intention of improving outcomes across the care continuum with multiple partners collaborating in their care, not on a single encounter associated with a fee-for-service transaction.
Providing exceptional value-based care demands understanding the populations served, the characteristics and needs of the population, and the individual, to develop the necessary interventions to improve health while managing care across the spectrum to produce the optimum results. What value-based care is not is an aggregation of services! Just because services exist within a single entity or location doesn’t mean there is accountability for care across the continuum or that care is integrated. The reality is without motivation to move beyond fee-for-service and to a value-based framework, there is no perceived need for accountability or integration. Connecticut is experiencing this exact situation. Without significant intervention and pressure to transition toward value, we should all expect a continued escalation in cost, with minimal to no improvement in quality of care.

Lisa Trumble, President and CEO